Dear World, please stay home. (That includes YOU, US Citizens.)
Hey everyone!! I hope you are doing well.
Unfortunately, though, I’m in quarantine, and I wanted to give you an overview of what is going on from my perspective.
I’m sick. But not horribly ill. At any other time, I wouldn’t even think about it; I would chalk it up to allergies and be on my way.
But, this isn’t allergies.
I was working March 13 and 14, which I’m glad I did to get all of the COVID19 prep done for my organization. But I also began to realize; I might be sick. On Saturday, I noticed I had a cough. Sunday morning, I noted some tension in my upper chest right around my collar bone.
On the morning of Sunday, March 15, I called the nurse hotline to discuss my symptoms. They asked me if I had recently traveled out of the country: no, I hadn’t. They asked me if I had been around someone who is a confirmed case of COVID19. I had to laugh. I said no. Only people that recently traveled overseas, or have been around a known COVID-19 carrier are tested. That’s quite a Catch-22. I explained where I work – at a public space right next to the Twin Cities International Airport, where people from all over the state and the world stop by to ask questions and enjoy the area I manage. I also have a PO Box in the St. Paul Post Office, located inside the Twin Cities International Airport, and I visit that space almost every day. They asked about my symptoms. I had a dry cough and chest tightness. They recommended I see a doctor in Urgent Care because of my chest tightness. After that call with the nurse, I started to feel my hands get cold. I recognized I was having a panic attack.
I’m temporarily living with my cousins since moving to the Twin Cities for a work promotion. My cousin, M., has asthma and is a breast cancer survivor. We’ve talked a lot about COVID-19 over the past month. She’s very much in the center of leadership for responding to the outbreak. She can’t afford to get sick. What if I’ve exposed her to the Coronavirus? I called my cousin to let her know I had a panic attack. She asked me why, and I told her, “I’m afraid I’m sick.” She told me, “It’s ok, my family has prepared for this. Go to the doctor ASAP.”
I saw a doctor in Urgent Care
I didn’t have a fever at the time my temp was 97.8, a typical temp for me. I only had a cough and chest tightness. He told me to go home and isolate. He also told me to get a COVID-19 test if my symptoms worsen.
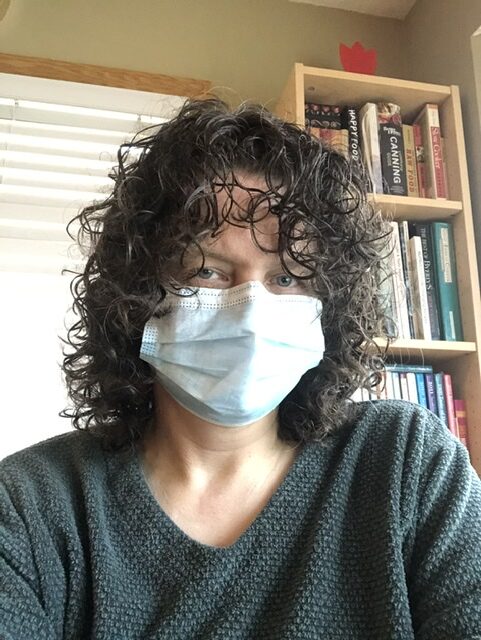
I called my cousin and let her know I was coming home from work early, and the doctor recommended I go into sequestration. My cousins headed out to the grocery stores to pick up last-minute perishables so we could shutter their home for a long time.
When I got home, I went directly to my room to get out of my work clothes. I felt guilty that I was possibly bringing something dangerous into their house. I was hopeful that everything was fine, and I just had allergies. My cousins and I talked about the next steps, and we started prepping to live separately within the house.
That evening I felt fine. My cough was just a little cough. As I got ready for bed, I checked for a fever, and sure enough, there it was: 100.1. I texted my cousins in the other part of the house, “SOB, I’m starting to run a fever, 100.1, I’ll go in for the test tomorrow morning.” M replied, “Sounds like a good plan.”
Had this cough happened during a regular spring, I would never have checked for a fever. I didn’t ache. I didn’t feel icky – was just a little tired, which I chalked up to staying up too late on my weekend without my son.
Testing
I went in for a COVID19 test on Monday, March 16, 2020, and I’m still waiting for results as of the writing of this article on March 25, 2020. I almost wasn’t allowed to get one. There was concern that there weren’t enough supplies. As of Monday, March 16, 2020, Minnesota was only testing people who had been in countries listed as having COVID-19 (primarily Japan, China, France, and Italy), or people who had been exposed to a known carrier of COVID-19.
When I arrived at the hospital, I stayed in my car and called the nurse hotline to request the test. I let the call-in nurse know that I couldn’t say if I had been exposed to a known carrier or not, but I work at a space close to the international airport that is often visitor’s first stop after arrival. I also informed the nurse that I live with someone with a compromised immune system. I asked the nurse if I could get tested for Influenza or Strep instead (to rule them out), and she let me know they stopped Influenza tests because they were running out of swabs (same swab for both tests), and I didn’t need a strep test. She discussed Influenza symptoms with me, and I didn’t have those. She said she would call the on-site COVID-19 scheduler and see if I could get a test.
I got the ok to have the test.
I hung up with the call-in nurse and waited for a return call. The COVID-19 scheduling nurse called me back and directed me to drive to a section of the parking lot where a tent was. As I drove over to the tent, the nurses waved me over to a parking spot. There was one other car waiting in the lot, and one car pulled up close to the tent. The nurses and the doctor were all wearing yellow disposable gowns, gloves taped to their sleeves, goggles, face shields, hair covers, and face masks. They were not changing their garments between tests.
A nurse walked out of the hospital to the tent with a folder. At the same time, I got a phone call telling me to pull up to the tent. A nurse and a doctor approached my car and verified who I was. Then the doctor swabbed my nose. The nurse gave me a COVID-19 quarantine handout and told me I should have the results in 3 days. She also said to me that everyone living in my household must follow the quarantine instructions. There wasn’t information on when I could stop quarantine, just what to do to be in quarantine. Back home, I went.
I’m hoping it’s negative, but behaving as if it’s positive.
Unfortunately, it’s likely I’ll never get my results because there aren’t enough supplies to conduct the test. As of Tuesday, March 17, 2020, the Minnesota Department of Health announced they are prioritizing tests for hospitalized patients, health care workers, and people living in group homes. I don’t fall into any of those categories.
I’m letting you know because this is very serious. Our health care providers don’t know how widespread this is or have the capacity to assess the magnitude. And – people like me are not going to get tested.
You don’t know if someone is sick by looking at them. People don’t even know they are sick. That first week, I felt fine. But I could infect many other people if I go out in public. As of Wednesday, March 18, 2020, the chest tightness has gotten more uncomfortable. I get winded, especially outside.
My fever hasn’t gone away since the evening of Sunday, March 15, 2020. The chest tightness and getting winded hasn’t gone away since March 18, 2020. The coughing comes and goes; it’s there every day.
I’m better off than many other people dealing with this illness. I know of another young woman who got sick two days before I did. Her fever is higher than mine, and she’s having more difficulty breathing than I am. She’s staying home, and she’s living with someone who can care for her. She couldn’t get the test.
I’m fighting it, and so far, I’m winning! But there have been some scary days. The worst was Monday, March 23, 2020.
On Monday, March 23, I woke up feeling good. I was tired and a bit winded, but my fever was down in the low 99’s. My cough felt like it was clearing something from my lungs. I sent a bunch of happy texts to my friends and family, letting them know I was feeling a lot better. I got online to work a little bit. As I pushed through emails, I noticed I was struggling to read them. Then I realized I was forgetting what I was doing. I worried I wasn’t catching information. I sent a text to my coworkers to let them know I felt compromised and wasn’t sure I was making correct decisions. I stopped working and went to my bedroom to lie down.
My cousin, J, FaceTimed me from the other part of the house. As we were talking, I felt sleepy and sometimes got lost in the conversation. My son would run in and out of the room, which kept me from falling asleep. My cousin was working as we were talking, so he didn’t see me get droopy. We finished our FaceTime, and I got out of bed. I walked into the kitchen and sat down to respond to a text. As I wrote the text, I felt like I was going to fall out of the chair. I hit send, but I wasn’t even sure if I finished my thought. I FaceTimed J to let him know I wasn’t feeling well. We started talking about what was going on, and I could tell I was struggling to get words to make sense. My cousins got ready to drive me to the ER and ended up calling the ambulance. Apparently, I started to look a little blue.
Ambulance
My chest was very tight, and breathing was difficult. I was super winded, and I was struggling to remember words. The EMTs arrived and talked to me for a while. It felt like forever; they had to ask if I had recently traveled to another country where COVID-19 was present or if I had known exposure to a COVID-19 patient. I had to tell them no.
They asked me how I was feeling and what was going on. I was standing and leaning on the couch for support as we talked. It felt like words were coming out of my mouth very slowly, and I had to pause to think about what word came next.
The EMTs asked me where I wanted to go. I had no idea. Thankfully my cousin is very familiar with the health care system in the Twin Cities and told them to take me to Regions Hospital, which is in-network for my insurance. I was able to walk to the ambulance and climb in without assistance.
As we drove to the hospital, the nurse asked me more questions about my health. I let her know that I have an underlying heart condition called Prinzmetal’s Angina. She hadn’t heard of it, so I explained that it’s a genetic condition, not easily diagnosed because it doesn’t usually show up on an EKG. The heart spasms spontaneously, usually while resting, and those spasms go away after a minute or two. It kind of hurts, but you rest a while and then go on with your day. Prinzmetal’s Angina is treated with nitroglycerin, which causes the heart muscle to relax.
She asked me how my heart was feeling, and I told her I really couldn’t tell – my chest felt tight. She said my heart rate was over 100 when I got into the ambulance, but it had slowed to 70 during the ride. It was comforting to know my heart wasn’t continuing to race. I had a hard time keeping my eyes open and my chest hurt quite a bit, though it wasn’t steady, it came in irregular pulses. As we drove to the ER, I did notice the pulses slowed down, and my vision and thoughts were becoming clearer.
She called ahead to the ER to let them know we were on our way, and they had a potential COVID19 case. The ER nurse told her to bring me into the vestibule, but not inside the ER. They would come and get me. The EMTs took me out of the ambulance and rolled me into the vestibule, and we waited. We waited for quite a while. The female EMT finally knocked on the window facing the ER desk. A nurse came over and looked in at us and pointed to a phone. The EMT picked up the phone and explained to the nurse that they were instructed to wait in the vestibule until one of them came to get me. The nurse told the EMT that they could just bring me in – a room was ready for me, and she apologized for the confusion. The EMTs brought me into my room, and I was able to walk from the stretcher to the hospital bed without assistance.
The doctors checked my lungs and heart.
I do have an underlying heart condition called Prinzmetal’s Angina, which the doctor treated with nitroglycerin. My heart muscle relaxed, the pain subsided, and my breathing got a lot better.
My lungs are clear, there’s no pneumonia, and if I do have Coronavirus, it’s not settling into my lungs, which is excellent!!
I asked them if they knew how the cycle works for the Coronavirus. How long does the illness last? Does it get worse and then better? They said typically symptoms get worse during days 7-13 (which is the timing I’m in), and then things will get better. Those that are hospitalized and become critical usually go on ventilators between days 7-13. Even with mild symptoms, it can last a few more weeks.
So – now I hope I’ve turned the corner for the better!! I’m super glad to know my lungs are clear and that my heart is fine.
I have an inhaler I can use every 4 hours, and they told me to take my nitroglycerin if the pain comes back.
But having the results of my COVID-19 test would make it much easier to know exactly what to do. And so I wait.
Love you all!!
I care about you all very much and want you to be safe.
Big virtual socially distant hugs to all of you!!
Author’s Note: After this article was done, the morning of March 26, I received the email letting me know I was COVID-19 negative. I’m still sick, but relieved and will continue social distancing. I’m on the upswing, but the fever still creeps up in the afternoon and the chest congestion lingers. I’m still new to understanding my heart condition and have learned to listen to my heart better and recognize the symptoms of distress. My thoughts are with the healthcare workers, and wish health upon the world.